Benadryl, Unisom, and ZzzQuil: The Same Product in Disguise—And Why They Aren’t Great for Sleep
If you’ve ever wandered the pharmacy aisles in search of a sleep aid, you’ve likely come across three popular over-the-counter options: Benadryl, Unisom, and ZzzQuil. Although marketed differently, these products often contain the same active ingredient—diphenhydramine (National Library of Medicine, 2022).
So, if they all share the same active ingredient, does that mean diphenhydramine is a good option for sleep? Not necessarily. In fact, medical experts do not recommend it for long-term sleep management (Qaseem et al., 2016). Let’s examine why.
What Is Diphenhydramine?
Diphenhydramine is a first-generation antihistamine initially developed for treating allergic reactions. It works by blocking histamine, a chemical that plays a key role in immune responses (National Library of Medicine, 2022). One of its most notable side effects is drowsiness, which is why it is marketed as a nighttime sleep aid.
However, despite its sedative properties, diphenhydramine is not recommended for long-term treatment of sleep disorders or chronic insomnia (Wilson et al., 2010).

Why Diphenhydramine Isn’t Ideal for Sleep
- It Disrupts Sleep Quality
Although it may help users fall asleep, diphenhydramine does not enhance the quality of sleep. Studies show it reduces the proportion of deep (slow-wave) sleep, leading to next-day grogginess and fatigue (Glass et al., 2005). - Tolerance Develops Quickly
Tolerance to the sedative effects of diphenhydramine can develop within just a few days, rendering it less effective over time. Increasing the dose to overcome this is not recommended due to safety concerns (Schutte-Rodin et al., 2008). - Long Half-Life Causes “Hangover” Effects
Diphenhydramine has a relatively long half-life (8–12 hours), which can lead to morning-after drowsiness, impaired cognitive function, and reduced alertness (Shahid et al., 2012). - Increased Risk in Older Adults
The American Geriatrics Society (AGS) strongly advises against the use of diphenhydramine in older adults due to increased risks of cognitive decline, dizziness, falls, and confusion (AGS Beers Criteria Update Expert Panel, 2019). - Potential Long-Term Side Effects
Long-term use has been linked to anticholinergic side effects, such as dry mouth, urinary retention, constipation, and even increased risk of dementia with chronic exposure (Gray et al., 2015).

Better Alternatives for Sleep
If you’re experiencing sleep difficulties, there are safer, more effective strategies supported by clinical research:
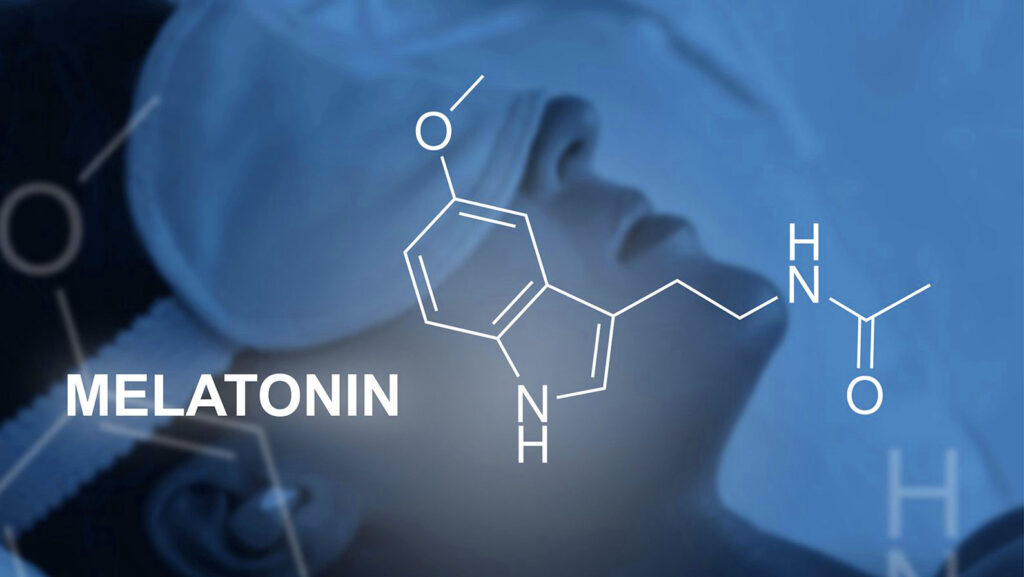
- Melatonin: A hormone that helps regulate circadian rhythms and is especially useful for jet lag or shift work (Ferracioli-Oda et al., 2013).
- Cognitive Behavioral Therapy for Insomnia (CBT-I): Considered the first-line treatment for chronic insomnia with long-term benefits (Trauer et al., 2015).
- Sleep Hygiene: Practicing good sleep habits—such as reducing screen time before bed, keeping a consistent sleep schedule, and avoiding caffeine—can significantly improve sleep.
- Magnesium and Valerian Root: Some natural supplements, like magnesium or valerian root, may promote relaxation and improve sleep quality, though more research is needed (Lindholm et al., 2021; Bent et al., 2006).
Final Thoughts
Benadryl, Unisom, and ZzzQuil are essentially the same medication in different packaging. While they may induce short-term drowsiness, they are not suitable for long-term management of sleep problems due to tolerance, next-day grogginess, reduced sleep quality, and long-term health risks—particularly in older adults.
If you’re struggling with persistent sleep issues, focus on evidence-based approaches and speak with a healthcare provider to explore safer, more sustainable treatment options.
Just because something is marketed for sleep doesn’t mean it’s the best tool for the job.
References
AGS Beers Criteria Update Expert Panel. (2019). American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 67(4), 674–694. https://doi.org/10.1111/jgs.15767
Bent, S., Padula, A., Moore, D., Patterson, M., & Mehling, W. (2006). Valerian for sleep: A systematic review and meta-analysis. American Journal of Medicine, 119(12), 1005–1012. https://doi.org/10.1016/j.amjmed.2006.02.026
Ferracioli-Oda, E., Qawasmi, A., & Bloch, M. H. (2013). Meta-analysis: Melatonin for the treatment of primary sleep disorders. PLoS ONE, 8(5), e63773. https://doi.org/10.1371/journal.pone.0063773
Glass, J., Lanctôt, K. L., Herrmann, N., Sproule, B. A., & Busto, U. E. (2005). Sedative hypnotics in older people with insomnia: Meta-analysis of risks and benefits. BMJ, 331(7526), 1169. https://doi.org/10.1136/bmj.38623.768588.47
Gray, S. L., Anderson, M. L., Dublin, S., Hanlon, J. T., Hubbard, R. A., Walker, R., … & Larson, E. B. (2015). Cumulative use of strong anticholinergics and incident dementia: A prospective cohort study. JAMA Internal Medicine, 175(3), 401–407. https://doi.org/10.1001/jamainternmed.2014.7663
Lindholm, C., Bellocco, R., & Lagerros, Y. T. (2021). Magnesium intake and sleep disorders: Findings from the Swedish National Diet Survey. Nutrients, 13(3), 842. https://doi.org/10.3390/nu13030842
National Library of Medicine. (2022). Diphenhydramine. MedlinePlus. https://medlineplus.gov/druginfo/meds/a682539.html
Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 165(2), 125–133. https://doi.org/10.7326/M15-2175
Schutte-Rodin, S., Broch, L., Buysse, D., Dorsey, C., & Sateia, M. (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 4(5), 487–504. https://doi.org/10.5664/jcsm.27286
Shahid, A., Wilkinson, K., Marcu, S., & Shapiro, C. M. (2012). STOP, THAT and One Hundred Other Sleep Scales. Springer.
Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., & Cunnington, D. (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191–204. https://doi.org/10.7326/M14-2841
Wilson, S. J., Nutt, D. J., Alford, C., Argyropoulos, S. V., Baldwin, D. S., Bateson, A. N., … & Wafford, K. A. (2010). British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. Journal of Psychopharmacology, 24(11), 1577–1600. https://doi.org/10.1177/02698811003761441




