Migraine and Sleep: A Complicated Relationship
Migraines are more than just headaches—they are a neurological condition that can significantly impact quality of life. Among the many factors that influence migraine frequency and severity, sleep plays one of the most crucial roles. Understanding how sleep and migraines are interconnected can help patients manage both more effectively.
The Sleep-Migraine Connection
Sleep and migraines share a bidirectional relationship. This means not only can poor sleep trigger migraines, but migraines themselves can disrupt sleep. Here’s how:

1. Poor Sleep Can Trigger Migraines
Sleep deprivation, irregular sleep schedules, or even oversleeping can all trigger migraines. This may be due to disruptions in brain chemicals like serotonin and dopamine, which are involved in both sleep regulation and migraine pathways.

2. Migraines Can Disrupt Sleep
- During a migraine attack, many patients experience difficulty falling or staying asleep due to pain, nausea, and sensitivity to light and sound. This fragmented sleep can worsen the frequency or intensity of future attacks.

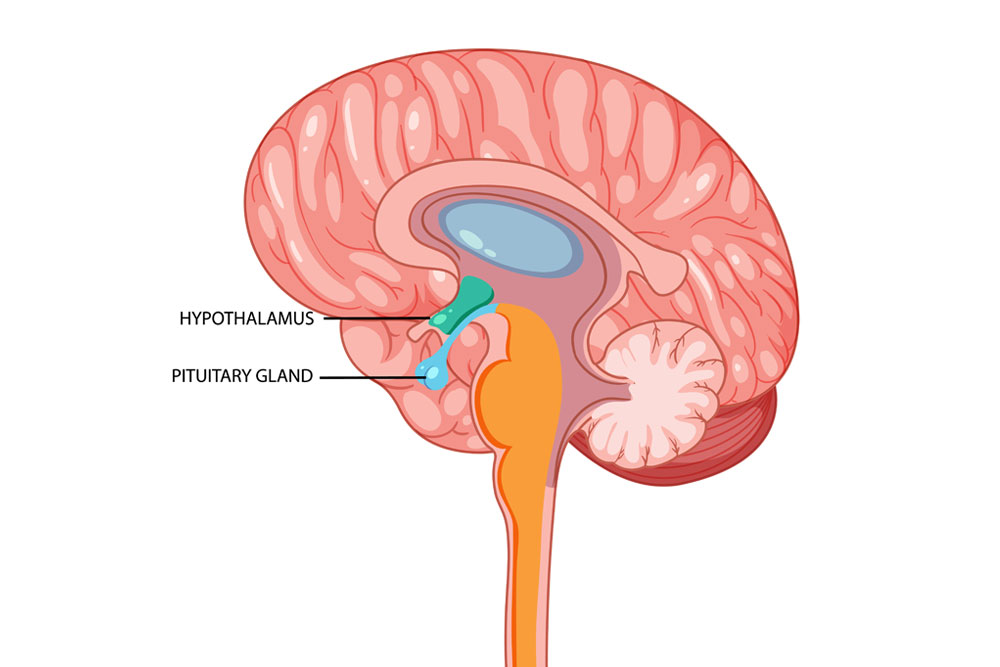
3. Shared Neurological Pathways
Both sleep and migraine regulation involve similar areas of the brain, such as the hypothalamus. Dysfunction in this region may explain why people with migraines often have comorbid sleep disorders, such as insomnia or restless legs syndrome.
Common Sleep Disorders in Migraine Sufferers
People with migraines are more likely to experience:
- Insomnia: Difficulty falling or staying asleep.
- Sleep apnea: A condition where breathing repeatedly stops and starts during sleep, leading to poor sleep quality.
- Restless Legs Syndrome: Uncomfortable sensations in the legs that interfere with sleep.
Hypersomnia: Excessive daytime sleepiness, sometimes from disrupted nighttime rest.

Tips for Better Sleep (and Fewer Migraines)
Improving sleep hygiene can help reduce migraine frequency and improve overall quality of life. Here are some strategies:
- Stick to a consistent sleep schedule, even on weekends.
- Create a calming bedtime routine—read, stretch, or meditate before bed.
- Avoid screens and bright lights at least an hour before sleep.
- Limit caffeine and alcohol, especially in the evening.
- Keep your bedroom cool, dark, and quiet.
- Exercise regularly, but avoid intense activity close to bedtime.

When to Seek Help
If you experience frequent migraines and suspect poor sleep may be playing a role, speak with your healthcare provider. A sleep study may be recommended if sleep apnea is suspected. In some cases, cognitive-behavioral therapy for insomnia (CBT-I) or medications that address both sleep and migraine symptoms may be beneficial.

The Bottom Line
Sleep and migraine management go hand-in-hand. While there’s no one-size-fits-all solution, improving sleep habits can lead to fewer migraine days and better overall well-being. If you’re struggling with both, addressing your sleep could be a vital step toward relief.
References (APA 7th Edition)
- Kelman, L., & Rains, J. C. (2005). Headache and sleep: Examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache: The Journal of Head and Face Pain, 45(7), 904–910. https://doi.org/10.1111/j.1526-4610.2005.05159.x
- Rains, J. C. (2018). Sleep and migraine: Assessment and treatment of comorbid sleep disorders. Headache: The Journal of Head and Face Pain, 58(7), 1074–1091. https://doi.org/10.1111/head.13355
- Ong, J. C., Park, M., Babson, K., & Finan, P. (2012). Sleep and pain. Pain Management, 2(5), 411–427. https://doi.org/10.2217/pmt.12.45
Lin, M., Lee, S. H., & Kim, H. J. (2022). Associations of poor sleep with migraine: A population-based study. Journal of Clinical Neurology, 18(1), 52–59. https://doi.org/10.3988/jcn.2022.18.1.52



